In the previous article , we review how hypertension and Obstructive sleep apnea (OSA) is closely associated with epidemiology and common clinical similarities in patients. In this article, we further discuss the pharmacological treatment guidelines for managing blood pressure (BP), including baseline patient evaluation of historical features favoring hypertension cause, laboratory tests for diagnostic procedures, pharmacological BP treatments, and drug response monitoring.
Patient screening for initiation of pharmacological treatment
In 2017, the American College of Cardiology / American Heart Association Task Force (1) published Clinical Practice Guidelines for patient evaluation in primary and secondary hypertension. Primary hypertension was defined by: i) a gradual increase in BP, with a slow rate of rise in BP, ii) lifestyle factors that favor higher BP (e.g., weight gain, high-sodium diet, decreased physical activity, excessive consumption of alcohol) and iii) family history of hypertension. On the other hand, secondary hypertension can be attributed to pheochromocytoma, OSA, chronic kidney disease due to post-renal urinary tract obstruction, hyperthyroidism, Cushing’s syndrome, medication and substance use.
Basic laboratory tests for primary hypertension should include fasting blood glucose, complete blood count, lipid profile, serum creatinine with eGFR, serum sodium, potassium, calcium, thyroid-stimulating hormone, urinalysis, and electrocardiogram.
Initiation of Pharmacological BP Treatment
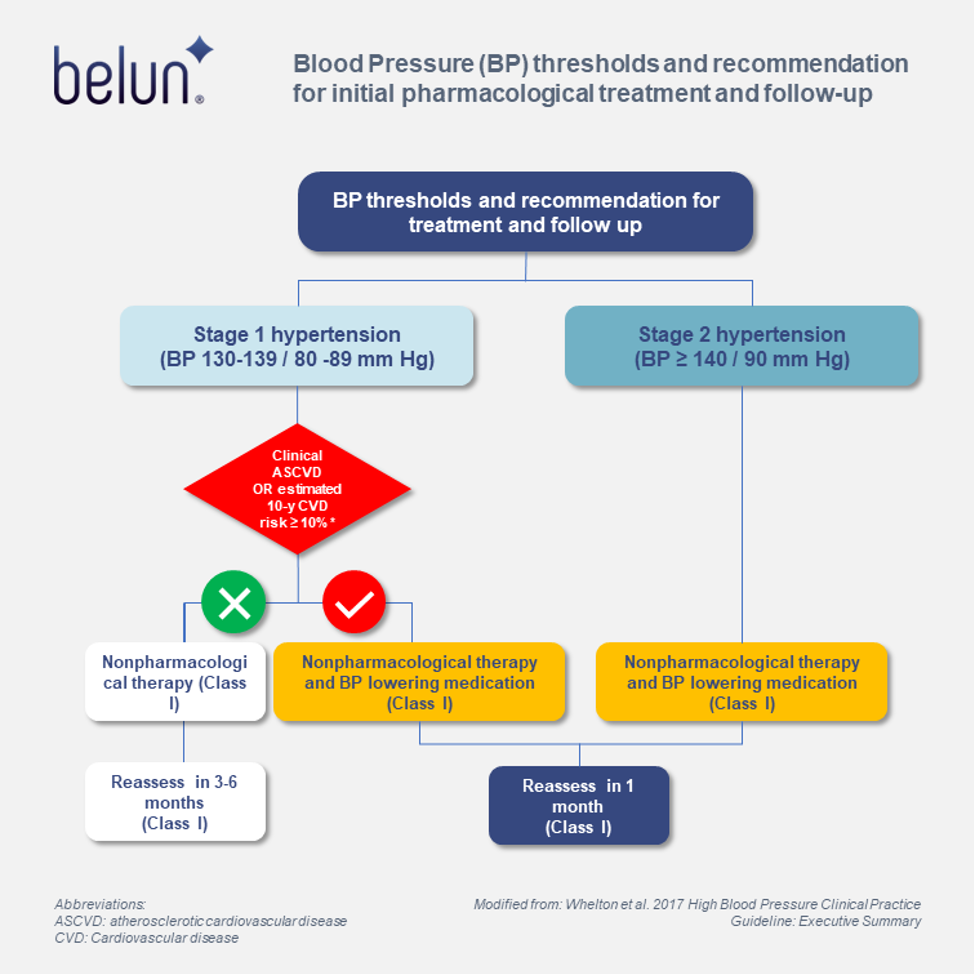
The use of BP-lowering medications is recommended for secondary prevention of recurrent Cardiovascular disease (CVD) events in patients with clinical CVD and an average SBP ≥ 130 mm Hg or an average DBP ≥ 80 mm Hg, and for primary prevention in adults with an estimated 10-year atherosclerotic cardiovascular disease (ASCVD) risk of ≥ 10% and average SBP ≥ 130 mm Hg or an average DBP ≥ 80 mm Hg.
The use of BP-lowering medication is also recommended for primary prevention of CVD in adults with no history of CVD and with an estimated 10-year ASCVD risk < 10% and an SDP ≥ 140 mm Hg or a DBP ≥ 90 mm Hg. The pictorial workflow on the thresholds for treatment and follow-up is demonstrated in figure 1.

Follow-up after initial BP evaluation
Guidelines for Follow-up after initial BP Evaluation are recommended as follows:
- For adults with normal BP, yearly evaluation is suggested.
- Adults with elevated BP or stage 1 Hypertension with ASCVD risk < 10% should be managed by nonpharmacological treatment and review BP within 3-6 months.
- Adults with stage 1 hypertension with ASCVD risk of ≥ 10% should be first managed by a combination of nonpharmacological and antihypertensive drug therapy and a repeat BP evaluation in 1 month.
- Adults with stage 2 hypertension should be evaluated or referred to a primary care provider within 1 month for initial diagnosis, provide nonpharmacological and antihypertensive drug therapy, and repeat evaluation within 1 month.
- For adults with high BP (e.g., SBP ≥ 180 mm Hg or DBP ≥ 110 mm Hg), evaluation should be immediate with antihypertensive drug treatment.
Appropriate follow-up and monitoring enable assessment of adherence and response to therapy; it also helps to identify adverse events by treatment and possible target organ damage and allows assessment of progress toward treatment goals.
A systematic approach to out-of-office BP assessment is an important part of follow-up and monitoring of BP to assess response to treatment, elimination of white coat hypertension, and detection of masked hypertension or uncontrolled hypertension.
How precision treatment in OSA can improve coexisting Resistant Hypertension
Although improvement of sleep was documented to have a modest effect on BP reduction, however, precision medicine may shed new light on targeting tailored-made treatment strategies for selecting responders to OSA treatment. Torre et al. conducted an interesting study to identify 84 micro-ribonucleic acid (miRNA) arrays that could predict blood pressure responses to CPAP treatment (2). The study participants were recruited in a relatively large, randomized, controlled trial from 24 Spanish teaching hospitals of patients with Resistant Hypertension (RH) and OSA. After performing miRNA PCR array-based expression analyses, a subset of 3 differentially expressed miRNAs were found to be predictive in the reduction of blood pressure after CPAP treatment. The panel provided a discriminatory predictive model for identifying responders and non-responders to CPAP treatment effective in BP reduction. The identification of responders to CPAP with BP reduction helps clinicians to customize CPAP treatment options for responders and perhaps provides evidence to suggest other OSA treatment options to non-responders (e.g., Mandibular advancement device).
How Belun can facilitate preventive management in Hypertension
Belun® remoVital remote monitoring system is a real-time monitoring system composed of an FDA 510(k)-cleared Belun® Ring and a communication hub. The system measures vital signs, including blood oxygen saturation, pulse rate, and body temperature. The installation is simple, user-friendly, and no pairing for Bluetooth or WiFi is required. The automatic connection with the cellular networks enables the system to run once it is turned on. It allows easy access to patients’ real-time measurements via the web portal. Besides, this real-time alarm customization alerts healthcare professionals if any measured vital sign exceeds the pre-set thresholds. RemoVital provides real-time monitoring of hypertensive patients with a high prevalence of underlying cardiovascular problems, which may require regular monitoring of vital signs.
Belun Sleep System (BSP) has the capability of monitoring and analyzing SpO2, heart rate variability (HRV), photoplethysmography (PPG) waveform, and accelerometer-derived actigraphy data. It can calculate an estimated apnea-hyponea index (bAHI). It can also differentiate wakefulness from sleep, perform sleep stage analysis and give REM and NREM sleep duration using its artificial intelligence platform. Furthermore, autonomic nervous system (ANS) activities, including sympathetic and parasympathetic activities, throughout the monitoring period. Belun Sleep System provides objective sleep impairments data that can monitor the treatment responses of patients with coexisting OSA and hypertension.
Going forward, Belun Sleep System herein serves to provide a cost-effective, readily available, automated, no-skilled technician-needed solution to cardiologists, sleep physicians, and patients with sleep-related disordered breathing population-wide. Besides, we empower physicians to have a brief overview of their vital signs, sleep problems, and cardiovascular health remotely in hypertensive patients with OSA before thorough medical examinations.

See more about how Dr. Chi-Hang Ronald Lee & his team in Singapore brings new management to hypertension patients with Belun® Ring. It demonstrates a new application & potential contributions of Belun Sleep System in screening OSA to hypertension patients with cardiovascular risks.
https://www.linkedin.com/feed/update/urn:li:activity:7051134960425947139
Partnering with Belun :
Up to now, over a hundred organizations, including HK hospital authority hospitals, medical groups, clinic groups, dentists, and elderly centers selected to use the Belun Sleep System, Belun® Ring and Sleep App, and Belun® remoVital monitoring system. Many doctors read our medical journal papers, including:
1) “Belun® Ring Platform: a novel home sleep apnea testing system for assessment of obstructive sleep apnea” (https://jcsm.aasm.org/doi/10.5664/jcsm.8592),
2) “Detection of obstructive sleep apnea using Belun Sleep Platform wearable with neural network based algorithm and its combined use with STOP-Bang questionnaire” (https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0258040),
3)Belun® Ring (Belun Sleep System BLS-100): Deep Learning-Facilitated Wearable Enables OSA Detection, Apnea Severity Categorization, and Sleep Stage Classification in Patients Suspected of OSA (https://journals.lww.com/jhypertension/Abstract/2023/06000/The_Belun_sleep_platform_to_diagnose_obstructive.16.aspx),
4) Correlation of Pulse Rate Variability(PRV) and Heart Rate Variability(HRV) Metrics During Sleep in Subjects Suspected of OSA (Accepted in SLEEP conference 2023, Abstract ID: 954).
If you would like to know more about how to adopt Belun’s solution in your organization or home use, please feel free to contact us to schedule a meeting by filling out the form below:
Your message has been sent
References
1. Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018 Jun;71(6):1269–324.
2. Sánchez-de-la-Torre M, Khalyfa A, Sánchez-de-la-Torre A, Martinez-Alonso M, Martinez-García MÁ, Barceló A, et al. Precision Medicine in Patients With Resistant Hypertension and Obstructive Sleep Apnea. Journal of the American College of Cardiology. 2015 Sep;66(9):1023–32.