Part 1 :
Advocated workflow for dental management in Sleep medicine
Management of sleep disorders is an expanding area in medical care, and in recent decades, dentists may play an important role in diagnosing and treating sleep disorders. In the previous article, we addressed the advocated guidelines provided by the American Academy of sleep medicine (AASM) and the American Academy of Dental Sleep Medicine (AADSM) for the treatment of Obstructive Sleep Apnea (OSA) and Snoring with Oral Appliance Therapy (OAT) (1), type of interventions for OSA treatment and comparable benefits using Oral Appliances (OAs) versus Continuous Positive Airway Pressure (CPAP). In this review, we will discuss the actual guidelines for short and long-term dental management, potential factors contributing to the success of OAT, and possible side effects in treating OSA.
Management in dental care for patients with suspected Sleep Related Disordered Breathing
Standards of Practice Committee of the AADSM suggested a management flowchart for dentists in 2018 (2). Two major pathways may lead to a dental patient’s evaluation of suspected sleep-related disordered breathing (SRDB). A patient may start a visit to a qualified dentist and be screened, or a physician may refer the diagnosed patient to a qualified dentist. The first visit to a qualified dentist should implement a screening process including nocturnal and daytime symptoms (e.g., snoring, witnessed apnea, gasping, sleepiness), STOP-BANG questionnaires, chief complaints, medical and family histories, current medications, dental history and findings. It is also important to record baselines such as BMI, blood pressure and neck circumference for OAT monitoring. Then in consultation with the patient, the qualified dentist should then refer the suspected case to a physician for evaluation and assessment of SRDB. Another pathway may be a physician who has diagnosed a patient with SRBD, referring the patient to a qualified dentist for dental assessment and initiation of OAT. Patients undergoing OAT should be educated on their SRBD severity, including AHI, RDI and REI from sleep test results. They should also be informed that OAT success may be affected by fragmented sleep, oxygen desaturation and other co-existing sleep problems. (2)

Clinical characteristics contributing to the success and failure of OAT
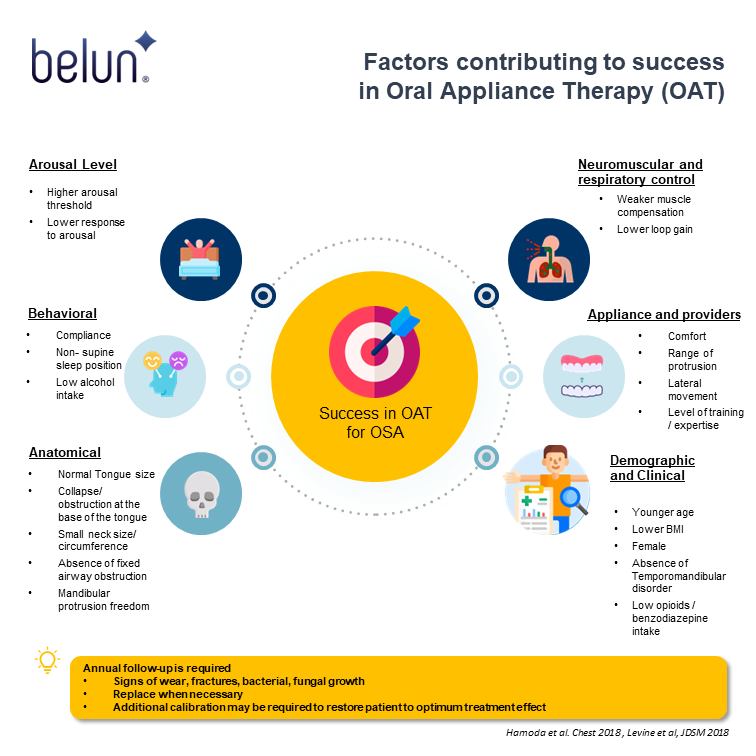
Evidence showed that OAT works better on anatomic traits by opening the airway, preventing closure and probably acting as a mandibular and tongue retainer. OA may help to reduce sleep arousals, effective in patients with low loop gain of ventilatory control reflex. Additional characteristics contributing to treatment efficiency are summarized in Figure 2 (3).
In the long term, patients who have higher respiratory arousal showed better improvement in sleepiness. Patients preferred OA as a first-time treatment or have complete symptom resolution may have higher adherence in the long run. From the perspective of OA fabrication and titration, the use of Bi-Bloc OA enabling relatively free mandibular movement or custom-made OA with regular dental follow-up showed better adherence. Regular follow-ups also help to minimize early side effects and treatment discontinuation. Support from bed partners by improving bed partners’ sleep quality is another important factor in OAT success (4).

Side effects and Contraindications of OAT
Side effects, such as dental pain, muscular pain, excessive salivation or dryness, may result in non-adherence (4). While bite change, dental and occlusal changes, mesial tipping of mandibular molars and distal tipping of maxillary molars, increased mandibular arch length, and downward rotation of mandible were reported. These changes are usually irreversible (5–11). Although side effects may seem substantial, patients should not discontinue the OAT unless there is a better treatment option provided since the preventive benefits of life-threatening outcomes of OSA outweigh the side effects of OAT.
It is also worth noting that edentulous patients with inadequate teeth, patients with severe periodontitis or a history of temporomandibular joint may not be suitable for OAT (12).
Calibration of OA and long-term management
In the previous decades for OAT, evidence on treatment effect and adherence with OA had been limited. In particular, adherence to OAT has recently been limited to self-reported data, with the inherent risks of overreporting (4). While extensive publications have been reported on the efficacy of short-term and long-term treatment of CPAP, the effectiveness and long-term adherence of OAT remain to be investigated. According to guidelines in 2015 (1), home sleep tests should be implemented for follow-up visits for treatment efficacy or even annual follow-ups to evaluate the long-term effects of OAT. Patients are expected to return to a qualified dentist within the first 30 days to assess the comfort and efficacy of the OAT. In addition, the qualified dentist will need to determine an appropriate endpoint for the OA advancement process. Consideration of evidence supporting 50% improvement in baseline AHI may be considered as partial treatment success (11). The AASM and American Medical Association (AMA) have published policies that a physician must order a home sleep apnea test to determine the appliance’s efficacy (13,14). Therefore the interpretation of sleep results should be in consultation with the qualified dentist, patient and physician. Additionally, final calibration of the OA, the qualified dentist should refer the patient back to the physician for assessment of OAT outcomes(2).
For long-term follow-up and management, patients are expected to follow up every 6 months for the first year and at least annually thereafter. The annual examination should include verification of OA efficacy and occlusal stability, check of the structural integrity of OA, symptoms evaluation, patient comfort and adherence rate,and possible short and long-term side effects (2). In case of damage, bacterial or fungal growth, replacement should be made, and additional calibration should be conducted (2).
How Belun can help
According to AASM and AMA published policies, a physician must order a home sleep apnea test to determine the efficacy of OAT. For long-term management, patients are expected to assess their sleep architecture at baseline, 1 month, 6 months, and yearly follow-ups to ensure good adherence and long-term prevention of life-threatening complications associated with OSA. For example, Belun Sleep Platform (BSP), using an FDA-cleared wearable Ring, offers an automated Home sleep test for patients with OSA.
Belun Sleep System (BSP) has the capability of monitoring and analyzing SpO2, heart rate variability (HRV), photoplethysmography (PPG) waveform, and accelerometer-derived actigraphy data. It can calculate an estimated apnea-hyponea index (bAHI). It can also differentiate wakefulness from sleep, perform sleep stage analysis and give REM and NREM sleep duration using its artificial intelligence platform. Furthermore, autonomic nervous system (ANS) activities, including sympathetic and parasympathetic activities, throughout the monitoring period. From the assessment provided by Belun Sleep System, objective sleep impairments data. Although polysomnography is currently the gold standard for measuring sleep quality, the test is costly, not easily available, and requires skilled sleep technicians for assessment. Going forward, Belun Sleep System herein serves to provide a cost-effective, readily available, automated, no-skilled technician-needed solution to dentists, sleep physicians, and patients with sleep-related disordered breathing population-wide.
Partnering with Belun :
Up to now, over a hundred organizations, including HK hospital authority hospitals, medical groups, clinic groups, dentists, and elderly centers selected to use the Belun Sleep System, Belun® Ring and Sleep App, and Belun® remoVital monitoring system. Many doctors read our medical journal papers, including:
1) “Belun® Ring Platform: a novel home sleep apnea testing system for assessment of obstructive sleep apnea” (https://jcsm.aasm.org/doi/10.5664/jcsm.8592),
2) “Detection of obstructive sleep apnea using Belun Sleep Platform wearable with neural network based algorithm and its combined use with STOP-Bang questionnaire” (https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0258040),
3)Belun® Ring (Belun Sleep System BLS-100): Deep Learning-Facilitated Wearable Enables OSA Detection, Apnea Severity Categorization, and Sleep Stage Classification in Patients Suspected of OSA (https://journals.lww.com/jhypertension/Abstract/2023/06000/The_Belun_sleep_platform_to_diagnose_obstructive.16.aspx),
4) Correlation of Pulse Rate Variability(PRV) and Heart Rate Variability(HRV) Metrics During Sleep in Subjects Suspected of OSA (Accepted in SLEEP conference 2023, Abstract ID: 954).
If you would like to know more about how to adopt Belun’s solution in your organization or home use, please feel free to contact us to schedule a meeting by filling out the form below:
Your message has been sent
References:
1. Clinical Practice Guideline for the Treatment of Obstructive Sleep Apnea and Snoring with Oral Appliance Therapy: An Update for 2015 [Internet]. [cited 2022 Sep 5]. Available from: https://jcsm.aasm.org/doi/epdf/10.5664/jcsm.4858
2. Levine M, Bennett K, Cantwell M, Postol K, Schwartz D. Dental Sleep Medicine Standards for Screening, Treating, and Managing Adults with Sleep-Related Breathing Disorders. J Dent Sleep Med. 2018 Jul 10;5(3):61–8.
3. Lavigne GJ, Herrero Babiloni A, Beetz G, Dal Fabbro C, Sutherland K, Huynh N, et al. Critical Issues in Dental and Medical Management of Obstructive Sleep Apnea. J Dent Res. 2020 Jan 1;99(1):26–35.
4. Tallamraju H, Newton JT, Fleming PS, Johal A. Factors influencing adherence to oral appliance therapy in adults with obstructive sleep apnea: a systematic review and meta-analysis. Journal of Clinical Sleep Medicine. 17(7):1485–98.
5. Aarab G, Lobbezoo F, Heymans MW, Hamburger HL, Naeije M. Long-Term Follow-Up of a Randomized Controlled Trial of Oral Appliance Therapy in Obstructive Sleep Apnea. RES. 2011;82(2):162–8.
6. Doff MHJ, Hoekema A, Pruim GJ, Huddleston Slater JJR, Stegenga B. Long-term oral-appliance therapy in obstructive sleep apnea: a cephalometric study of craniofacial changes. J Dent. 2010 Dec;38(12):1010–8.
7. Fransson AMC, Kowalczyk A, Isacsson G. A prospective 10-year follow-up dental cast study of patients with obstructive sleep apnoea/snoring who use a mandibular protruding device. Eur J Orthod. 2017 Oct 1;39(5):502–8.
8. Chen H, Lowe AA, de Almeida FR, Fleetham JA, Wang B. Three-dimensional computer-assisted study model analysis of long-term oral-appliance wear. Part 2. Side effects of oral appliances in obstructive sleep apnea patients. Am J Orthod Dentofacial Orthop. 2008 Sep;134(3):408–17.
9. Rose EC, Staats R, Virchow C, Jonas IE. Occlusal and skeletal effects of an oral appliance in the treatment of obstructive sleep apnea. Chest. 2002 Sep;122(3):871–7.
10. Pliska BT, Nam H, Chen H, Lowe AA, Almeida FR. Obstructive sleep apnea and mandibular advancement splints: occlusal effects and progression of changes associated with a decade of treatment. J Clin Sleep Med. 2014 Dec 15;10(12):1285–91.
11. Hamoda MM, Kohzuka Y, Almeida FR. Oral Appliances for the Management of OSA: An Updated Review of the Literature. Chest. 2018 Feb 1;153(2):544–53.
12. Ng JH, Yow M. Oral Appliances in the Management of Obstructive Sleep Apnea – Sleep Medicine Clinics [Internet]. [cited 2022 Sep 5]. Available from: https://www.sleep.theclinics.com/article/S1556-407X(18)30092-4/fulltext
13. Rosen IM, Kirsch DB, Chervin RD, Carden KA, Ramar K, Aurora RN, et al. Clinical Use of a Home Sleep Apnea Test: An American Academy of Sleep Medicine Position Statement. J Clin Sleep Med. 2017 Oct 15;13(10):1205–7.
14. H-35.963 Appropriate Use of Objective Tests for Obstructive Sle | AMA [Internet]. [cited 2022 Sep 10]. Available from: https://policysearch.ama-assn.org/policyfinder/detail/sleep%20apnea?uri=%2FAMADoc%2FHOD.xml-H-35.963.xml