Management of sleep disorders is an expanding area in medical care, and in recent decades, dentists may play an important role in diagnosing and treating sleep disorders. In addition, many dental complaints in a regular dental examination may be related to sleep quality. (e.g., Grinding teeth (Bruxism), dry mouth on awakening, morning headache, oral-facial pain symptoms, daytime sleepiness, loud or irregular snoring, and apnea reported by bed partners).
In 2015, the US cost of diagnosing and treating Obstructive Sleep apnea (OSA) was approximately US$12.4 billion (1,2). The Obstructive Sleep Apnoea Health Economics report by the British Lung Foundation suggests an estimated 1.5 million adults in the UK have sleep apnea, although only around 330,000 are currently diagnosed and treated (3).
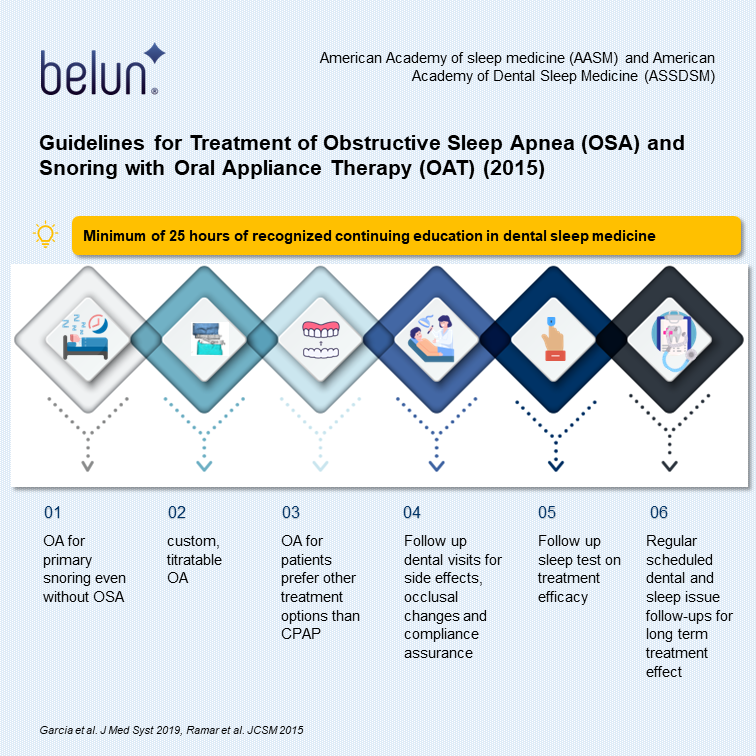
In the past decades, although 5.2% of dental patients were identified as high risk of OSA, none received a referral for further OSA evaluation (4). Furthermore, 54% of dentists never consulted a physician about a suspected OSA patient (5). In light of the growing prevalence and serious health outcomes associated with OSA, the American Academy of sleep medicine (AASM) and the American Academy of Dental Sleep Medicine (AADSM) published guidelines in 2015 for the treatment of Obstructive Sleep Apnea and Snoring with Oral Appliance Therapy (6), dentists are advocated as the frontiers in medical examinations for patients with potential sleep problems. Qualified dentists should have a minimum of 25 hours of recognized continuing education in dental sleep medicine (e.g., American Dental Association Continuing Education Recognition Program [ADA CERP] or Academy of General Dentistry Program Approval for Continuing Education [AGD PACE] ) provided by a dental sleep medicine focused non-profit organization or accredited dental school in the last two years. The major recommendations are as follows:
- Sleep physicians prescribe oral appliances, rather than no therapy, for adult patients who request treatment for primary snoring (without OSA)
- When oral appliance therapy (OAT) is prescribed by a sleep physician for an adult patient with OSA, a qualified dentist should use a custom, titratable appliance over non-custom oral devices
- Sleep physicians should consider prescriptions of an oral appliance (OA), rather than no treatment, for adults with OSA who are reluctant to use CPAP or prefer alternative therapy.
- Qualified dentists should provide oversight rather than no follow-up of OAT in adults with OSA to survey for dental-related side effects or occlusal changes and reduce their incidence.
- Sleep physicians should conduct follow-up sleep tests to improve or confirm treatment efficacy rather than follow-ups without sleep tests for patients fitted with OAs.
- Sleep physicians and qualified dentists should instruct adult patients with OAT for scheduled visits as opposed to no follow-up.
During the COVID-19 pandemic, OAT is even advocated as the first-line therapy for OSA (7) as it does not generate aerosols, is easily disinfected, and does not need replaceable parts, unlike Continuous positive airway pressure (CPAP), which experienced a shortage of supplies during the COVID lockdown. Patients who prefer OAT may be more likely to adhere to the treatment since it does not increase the significant risk of COVID-19 exposure (7).

Types of interventions to treat OSA
While not all patients may be suitable for OA use, several available treatment options are available for patients with OSA. For example, it could be pharmacological to use domperidone and pseudoephedrine to reduce snoring; however, the effectiveness of therapy was not substantially validated with limited evidence (8). Surgery has been advocated to address structural issues, but NICE guidelines state that there is a lack of evidence of the clinical effectiveness of surgery for OSA; thus, it is not routinely used (9). Given the non-invasive, cost-effective, reversible nature of OAs, they are recommended as useful devices to treat mild to moderate OSA. OAs were mainly categorized into the following types: custom titratable; custom, non-titratable; non-custom, titratable; and non-custom, non-titratable. The guidelines in 2015 recommended the use of custom, titratable appliances as the best type of OA for OSA treatment.
Comparable Benefits using OAs vs CPAP
CPAP and OAs can reduce upper airway collapse during sleep, with CPAP having great efficacy in moderate to severe OSA. CPAP reduces the apnea-hypopnea index (AHI), respiratory disturbance index (RDI), or respiratory event index (REI) more than OAs in adult patients with moderate OSA (6). However, there are no significant differences in quality of life and cognitive and functional outcomes (10). Interestingly, it is worth noting that adherence to CPAP is generally lower than OA. Moreover, greater efficacy of CPAP may not necessarily translate into better treatment outcomes. In various randomized control trials comparing CPAP to OA across various severity of OSA patients, the use of CPAP and OA showed comparable results in improving symptoms of sleepiness (11,12), quality of life (13), and drive performance (14), cardiovascular outcomes and short-term effects on blood pressure (15) and even mortality rate in patients with severe OSA (16,17). The possible reason for the similar treatment effect between CPAP and OA was due to the longer adherence to OA compared to CPAP by patients. The adverse side effects, such as pressure sores, mask dislodgement, claustrophobia, air leakage, and nasal congestion had made CPAP intolerable to many patients (18). About 20-50% of OSA patients are reluctant to comply with CPAP (19), and adherence with CPAP is reportedly over 1h/night lower than OA (14). Moreover, OAT was also reported to be effective in two-thirds of patients after 3 years of treatment (20). Combination therapy of CPAP and OA was thus advocated to reduce the upper airway resistance and allow a more comfortable and lower pressure to sustain patency of the airway (21). The benefits of OAT are summarized in the figure below.

How Belun can facilitate OAT
According to AASM and American Medical Association published policies, a physician must order a home sleep apnea test to determine the efficacy of OAT. For long-term management, patients are expected to assess their sleep architecture at baseline, 1 month, 6 months, and yearly follow-ups to ensure good adherence and long-term prevention of life-threatening complications associated with OSA. For example, Belun Sleep System (BSP), using an FDA-cleared wearable Ring, offers an automated Home sleep test for patients with OSA.
Belun Sleep System (BSP) has the capability of monitoring and analyzing SpO2, heart rate variability (HRV), photoplethysmography (PPG) waveform, and accelerometer-derived actigraphy data. It can calculate an estimated apnea-hyponea index (bAHI). It can also differentiate wakefulness from sleep, perform sleep stage analysis and give REM and NREM sleep duration using its artificial intelligence platform. Furthermore, autonomic nervous system (ANS) activities, including sympathetic and parasympathetic activities, throughout the monitoring period. From the assessment provided by Belun Sleep System, objective sleep impairments data. Although polysomnography is currently the gold standard for measuring sleep quality, the test is costly, not easily available, and requires skilled sleep technicians for assessment. Going forward, Belun Sleep System herein serves to provide a cost-effective, readily available, automated, no-skilled technician-needed solution to dentists, sleep physicians, and patients with sleep-related disordered breathing population-wide.
Continued Reading :
Partnering with Belun :
Up to now, over a hundred organizations, including HK hospital authority hospitals, medical groups, clinic groups, dentists, and elderly centers selected to use the Belun Sleep System, Belun® Ring and Sleep App, and Belun® remoVital monitoring system. Many doctors read our medical journal papers, including:
1) “Belun® Ring Platform: a novel home sleep apnea testing system for assessment of obstructive sleep apnea” (https://jcsm.aasm.org/doi/10.5664/jcsm.8592),
2) “Detection of obstructive sleep apnea using Belun Sleep Platform wearable with neural network based algorithm and its combined use with STOP-Bang questionnaire” (https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0258040),
3)Belun® Ring (Belun Sleep System BLS-100): Deep Learning-Facilitated Wearable Enables OSA Detection, Apnea Severity Categorization, and Sleep Stage Classification in Patients Suspected of OSA (https://journals.lww.com/jhypertension/Abstract/2023/06000/The_Belun_sleep_platform_to_diagnose_obstructive.16.aspx),
4) Correlation of Pulse Rate Variability(PRV) and Heart Rate Variability(HRV) Metrics During Sleep in Subjects Suspected of OSA (Accepted in SLEEP conference 2023, Abstract ID: 954).
If you would like to know more about how to adopt Belun’s solution in your organization or home use, please feel free to contact us to schedule a meeting by filling out the form below:
Your message has been sent
References:
1. Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Ip MSM, Morrell MJ, et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. The Lancet Respiratory Medicine. 2019 Aug 1;7(8):687–98.
2. Watson NF. Health Care Savings: The Economic Value of Diagnostic and Therapeutic Care for Obstructive Sleep Apnea. J Clin Sleep Med. 2016 Aug 15;12(8):1075–7.
3. Steier J, Martin A, Harris J, Jarrold I, Pugh D, Williams A. Predicted relative prevalence estimates for obstructive sleep apnoea and the associated healthcare provision across the UK. Thorax. 2014 Apr 1;69(4):390–2.
4. Guess NW, Fischbach H, Ni AA, Firestone AR. Referral rate for obstructive sleep apnea in a pre-doctoral dental clinic using the STOP-Bang Questionnaire. Journal of Dental Education. 2022;86(4):456–62.
5. Knowledge, opinions, and clinical experience of general practice dentists toward obstructive sleep apnea and oral appliances – PubMed [Internet]. [cited 2022 Sep 7]. Available from: https://pubmed.ncbi.nlm.nih.gov/15211392/
6. Clinical Practice Guideline for the Treatment of Obstructive Sleep Apnea and Snoring with Oral Appliance Therapy: An Update for 2015 [Internet]. [cited 2022 Sep 5]. Available from: https://jcsm.aasm.org/doi/epdf/10.5664/jcsm.4858
7. Schwartz D, Addy N, Levine M, Smith H. Oral appliance therapy should be prescribed as a first-line therapy for OSA during the COVID-19 pandemic. J Dent Sleep Med [Internet]. 2020 Jul 10 [cited 2022 Sep 5];7(3). Available from: https://www.aadsm.org/docs/jdsm.7.10.2020.sa1.pdf
8. Larrain A, Kapur VK, Gooley TA, Pope CE. Pharmacological treatment of obstructive sleep apnea with a combination of pseudoephedrine and domperidone. J Clin Sleep Med. 2010 Apr 15;6(2):117–23.
9. Tanna N, Smith BD, Zapanta PE, Karanetz I, Andrews BT, Urata MM, et al. Surgical Management of Obstructive Sleep Apnea. Plast Reconstr Surg. 2016 Apr;137(4):1263–72.
10. Schwartz M, Acosta L, Hung YL, Padilla M, Enciso R. Effects of CPAP and mandibular advancement device treatment in obstructive sleep apnea patients: a systematic review and meta-analysis. Sleep Breath. 2018 Sep;22(3):555–68.
11. Sharples LD, Clutterbuck-James AL, Glover MJ, Bennett MS, Chadwick R, Pittman MA, et al. Meta-analysis of randomised controlled trials of oral mandibular advancement devices and continuous positive airway pressure for obstructive sleep apnoea-hypopnoea. Sleep Med Rev. 2016 Jun;27:108–24.
12. Iftikhar IH, Bittencourt L, Youngstedt SD, Ayas N, Cistulli P, Schwab R, et al. Comparative efficacy of CPAP, MADs, exercise-training, and dietary weight loss for sleep apnea: a network meta-analysis. Sleep Med. 2017 Feb;30:7–14.
13. Gupta MA, Simpson FC, Lyons DCA. The effect of treating obstructive sleep apnea with positive airway pressure on depression and other subjective symptoms: A systematic review and meta-analysis. Sleep Med Rev. 2016 Aug;28:55–68.
14. Health outcomes of continuous positive airway pressure versus oral appliance treatment for obstructive sleep apnea: a randomized controlled trial – PubMed [Internet]. [cited 2022 Sep 9]. Available from: https://pubmed.ncbi.nlm.nih.gov/23413266/
15. CPAP vs Mandibular Advancement Devices and Blood Pressure in Patients With Obstructive Sleep Apnea: A Systematic Review and Meta-analysis | Cardiology | JAMA | JAMA Network [Internet]. [cited 2022 Sep 9]. Available from: https://jamanetwork.com/journals/jama/fullarticle/2473494
16. Anandam A, Patil M, Akinnusi M, Jaoude P, El-Solh AA. Cardiovascular mortality in obstructive sleep apnoea treated with continuous positive airway pressure or oral appliance: an observational study. Respirology. 2013 Nov;18(8):1184–90.
17. Hamoda MM, Kohzuka Y, Almeida FR. Oral Appliances for the Management of OSA: An Updated Review of the Literature. Chest. 2018 Feb 1;153(2):544–53.
18. Tallamraju H, Newton JT, Fleming PS, Johal A. Factors influencing adherence to oral appliance therapy in adults with obstructive sleep apnea: a systematic review and meta-analysis. Journal of Clinical Sleep Medicine. 17(7):1485–98.
19. Sawyer AM, Gooneratne NS, Marcus CL, Ofer D, Richards KC, Weaver TE. A systematic review of CPAP adherence across age groups: clinical and empiric insights for developing CPAP adherence interventions. Sleep Med Rev. 2011 Dec;15(6):343–56.
20. Attali V, Chaumereuil C, Arnulf I, Golmard JL, Tordjman F, Morin L, et al. Predictors of long-term effectiveness to mandibular repositioning device treatment in obstructive sleep apnea patients after 1000 days. Sleep Med. 2016 Dec;27–28:107–14.
21. Levine M, Bennett K, Cantwell M, Postol K, Schwartz D. Dental Sleep Medicine Standards for Screening, Treating, and Managing Adults with Sleep-Related Breathing Disorders. J Dent Sleep Med. 2018 Jul 10;5(3):61–8.